Written with contributing author Linda Robinson, MSN, CPXP, RN, Vice President of Clinical Excellence, MDM Healthcare
As June unfolds, we acknowledge the significance of Alzheimer's and Brain Awareness Month—a time dedicated to raising awareness about Alzheimer's disease and other forms of dementia that impact millions of individuals across the United States.
In this article, we delve into the topic of dementia care, highlighting insights from our recent PX Space podcast interview with renowned Dementia Care Specialist, Teepa Snow, MS, OTR/L, FAOTA. With her unique positive approach to dementia care, Snow offers valuable insights and strategies that can transform the caregiving experience and enrich the lives of both caregivers and those living with dementia. Snow is also the Owner and Founder of Positive Approach to Care®, an organization dedicated to enhancing the life and relationships of those living with brain change by fostering an inclusive global community. Snow’s personal mission is to better the lives of people with dementia—as well as the lives of their caregivers—by sharing what she has learned. An occupational therapist by training, today Snow stands out as a prominent global champion and educator, advocating for individuals affected by dementia or other cognitive impairments.

Snow explained why she decided to devote herself to dementia care.
“I had family members who developed dementia and I had friends who were figuring out how to support people living with dementia. I was working in a variety of settings where people living with dementia and their families were not getting what I considered good support, care information, or preparation and that’s not OK. So that got me on the road to thinking there are better ways to do this and it’s not fair that people and families don’t know that,” she said.
Snow has become a guiding light for caregivers and healthcare professionals seeking innovative ways to provide compassionate and effective dementia care. Her Positive Approach to Care™ (PAC) philosophy emphasizes the significance of connection, empathy, and person-centered care in supporting individuals with dementia. Through this approach, Snow focuses on recognizing and embracing the remaining abilities of individuals with dementia, rather than focusing solely on their limitations.
Snow firmly believes that education is the key to empowering caregivers. The diagnosis not only affects patients, but families as well. Snow pointed out that four out of five families fall apart due to dealing with the effects of this condition long term.
“This condition is devastating for families,” Snow explained. “Families often walk into the situation really unprepared to deal with more than the memory loss. However, dementia is an umbrella, it’s always more than memory. It’s judgement, problem solving, and changes in initiation,” she said.
In the interview, she discusses the importance of gaining an accurate understanding of dementia, its impact on brain function, and how to effectively communicate and connect with individuals living with dementia. By equipping caregivers with knowledge and practical skills, Snow enables them to navigate the challenges of caregiving with confidence and empathy, fostering a positive caregiving environment.

A cornerstone of Snow's approach is the concept of person-centered care. She emphasizes the need to recognize each person's unique abilities, preferences, and life experiences, allowing for personalized care that respects their individuality. Snow explains that caregivers can create an environment that promotes dignity, independence, and a sense of purpose for those living with dementia.
Communication can be a significant challenge when caring for someone with dementia. Snow shares valuable insights and techniques to enhance communication and meaningful engagement. Snow explained that the ideal skillset needed to communicate with memory care patients is often not properly taught. She gave the example of a patient being unable to recall the word restaurant: the patient says “the place where we go out to eat,” and the caregiver responds, “the place where we go out to eat, do you mean a restaurant or something else?”
Snow explains, “Instead of just giving them the word, you give them options to choose and that’s actually keeping their brain active, and it’s keeping people connected instead of flustered and confused. It’s better for the patient, but it’s also better for the caregiver as it turns out,” she said.
By adopting effective communication techniques, caregivers can reduce frustration, enhance relationships, and foster a sense of well-being for both the caregiver and the person with dementia.
Snow also encourages caregivers to focus on creating positive moments and joyful interactions throughout their caregiving journey. These moments can arise from engaging in meaningful activities and giving patients positive affirmations. Snow explained how impactful positivity is for dementia patients.
“The affirmation of ability is huge. You have to count the little wins. Finding those places and spaces to lift someone up, it actually makes their brain work better,” she said.
Snow expressed the healing power of celebrating these moments and fostering a positive atmosphere, caregivers can create a more fulfilling and enriching experience for themselves and their loved ones.

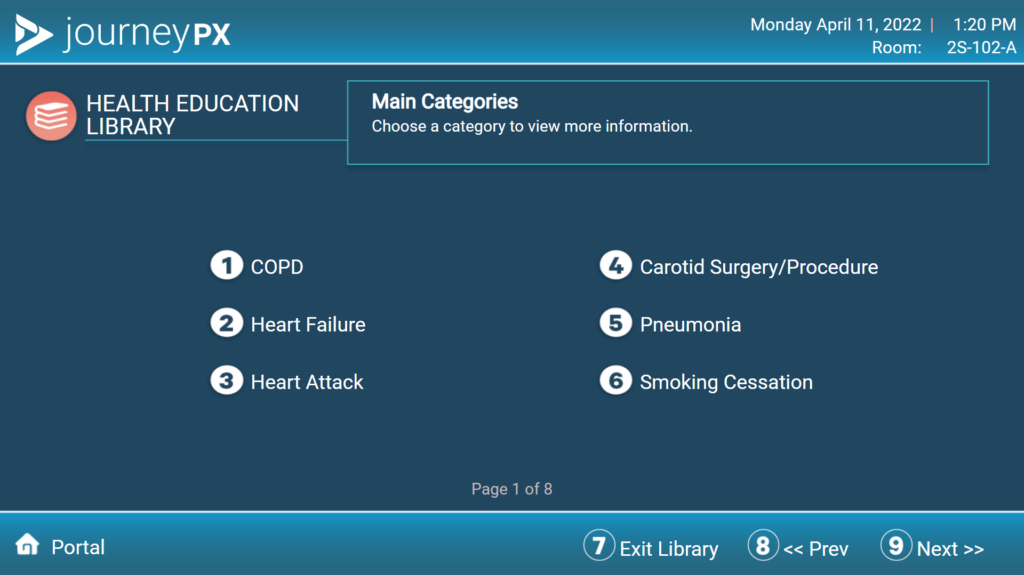
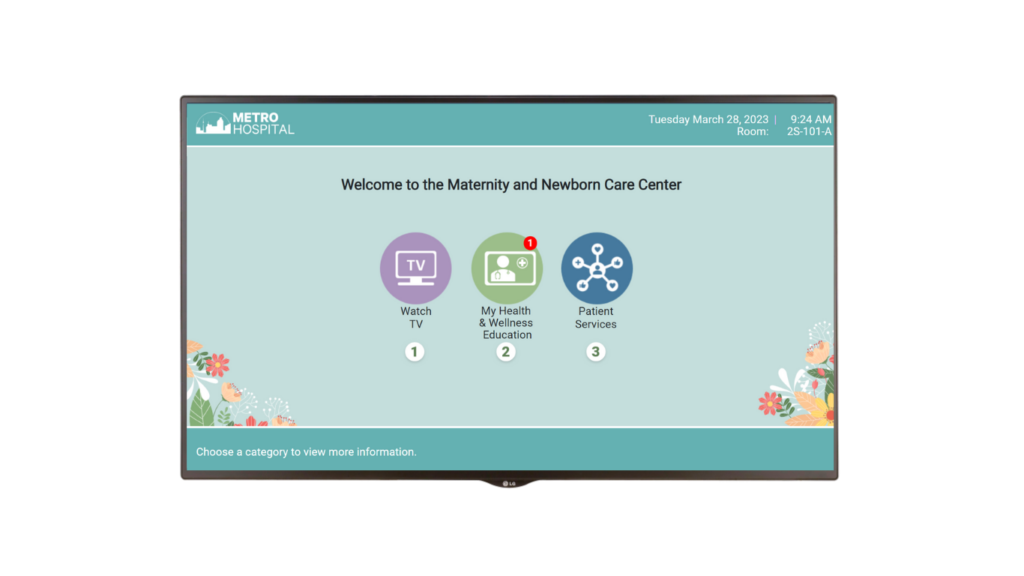
By emphasizing education, person-centered care, effective communication, and the creation of positive moments, Snow empowers caregivers to make a profound difference in the lives of those they care for. Empowering patients in their care journey is a philosophy embraced by innovative, cloud-based patient engagement platform Journey PX. Journey PX solutions empower patients by keeping them informed of their daily plan of care, providing individualized education, and streamlining communications between patients, families, and care teams. Journey PX’s digital whiteboard, My Day, Today, provides vital information to hospital care teams, patients, and their families. My Stay provides patients with the education they need via access to an extensive education library. This allows patients to become more empowered through health literacy and enhances their readiness for discharge. It also helps support patients after discharge by providing education that can be texted to them, giving an added layer of assurance that they will not be readmitted. Journey PX’s virtual care solution, Connect, is another piece of technology that supports the overall health and well-being of the patient, by allowing patients access to family members and care experts virtually at the bedside.

You can hear more from Teepa Snow by listening to the PX Space podcast interview. Also, learn more about her organization Positive Approach to Care® by visiting their website, contacting them at info@teepasnow.com, or calling 877-877-1671 for a consultation if you are a caregiver or family member of a memory care patient.