Written with the contributions of Linda Robinson, MSN, RN, CPXP, and Grace Schore
October marks National Physical Therapy Month, a dedicated time to recognize the pivotal role of physical therapy in patient care. With their expertise in strength training, core exercises, and a range of therapeutic techniques, physical therapists play a vital role in healing the body and enhancing well-being. They empower patients with invaluable tools to consider in their treatment journey, fostering holistic and effective approaches to recovery and preventive health. This month serves as a reminder of the profound impact physical therapy has on the lives of countless individuals seeking to improve their quality of life.
Linda Robinson, MSN, RN, CPXP, Vice President of Clinical Excellence at MDM Healthcare , recently hosted the dynamic physical therapy duo, Andrea Brogden, PT, DPT, and Amy Godfrey, PTA, on our podcast, PX Space.
Brogden and Godfrey, members of the dedicated team based at CORA Physical Therapy in Ponte Vedra Beach, Florida, collaborate to address their patients' physical limitations and concerns.
Brogden underscores the significance of understanding each patient's unique goals during the initial diagnosis.
"These goals can be as straightforward as the ability to comfortably roll out of bed, rise from a chair, or even run a marathon.”
She utilizes these goals as a guiding beacon, fostering a realistic perspective.
“We’re not aiming for a marathon next week; but let’s consider it six months down the road,” she said.
The team employs various metrics, including pain levels and incremental weekly objectives, alongside regular reassessments to monitor the patients’ advancements during their treatment.
"We assess factors such as range of motion, muscle strength, and overall mobility, all aligned with achieving those set objectives," Brogden noted.
One of the topics discussed was treating back pain, which, according to Brogden and Godfrey, is one of the primary concerns shared by those seeking treatment at their clinic.
“It is a very prevalent and common complaint reported by at least 65 million Americans. In fact, about 23% of the world's population suffers from back pain. Back pain can stem from something super mild to incredibly significant, and it can be very traumatic in our lives,” said Brogden.
As the evaluating therapist, Brogden's role is to determine the cause of pain. From there, she creates a treatment plan that Godfrey executes.
“We like to align the body first because when a patient is not in alignment, that can cause shooting pain into the lower or upper extremities. After we get everything aligned, we work on strengthening the core, starting with gentle exercises before progressing,” said Godfrey.
Godfrey discussed how she builds on the progress patients make with each session. As the treatment progresses, patients are gradually challenged to try some Pilates-inspired moves to build core strength.
Both Brogden and Godfrey agree that patients need to feel involved and in control of their treatment.
“I feel like that brings a lot of comfort to a patient, knowing where they are in the process and how we’re going to heal it,” said Brogden.
New tools have recently emerged to help patients in the office. Godfrey is trained in both Augmented Soft Tissue Manipulation (ASTYM) and Graston. These techniques find restrictions in soft tissue and can regenerate them at an accelerated rate. While stimulation was a popular technique in the past, Brogden noted that the team uses a range of techniques in their treatment plan, including dry needling. Dry needling is a technique similar to acupuncture, where small needles are inserted into muscle “trigger points” to relieve pain and irritation. Brogden has recently been certified in dry needling.

Brogden and Godfrey also emphasize patient education, recognizing the importance of keeping clients well-informed about their progress.
Brogden stressed the importance of teaching patients exercises that can be completed in their own homes. This is made easier with an online platform that includes videos on how to exercise correctly and information on the therapy’s benefits.
This is an invaluable tool for patients because good form and proper body mechanics are some of the biggest defenses against back pain. Brogden urged back pain sufferers to consider that daily movements can cause worsening damage if patients are not careful.
According to Godfrey, education is a key part of their patients’ success.
"We educate you from day one on proper body mechanics and proper form, then send you home with a home exercise program," she said.
Utilizing technology, patients have the capability to access their treatment plans from the comfort of their own homes, empowering them to take charge of their own recovery.

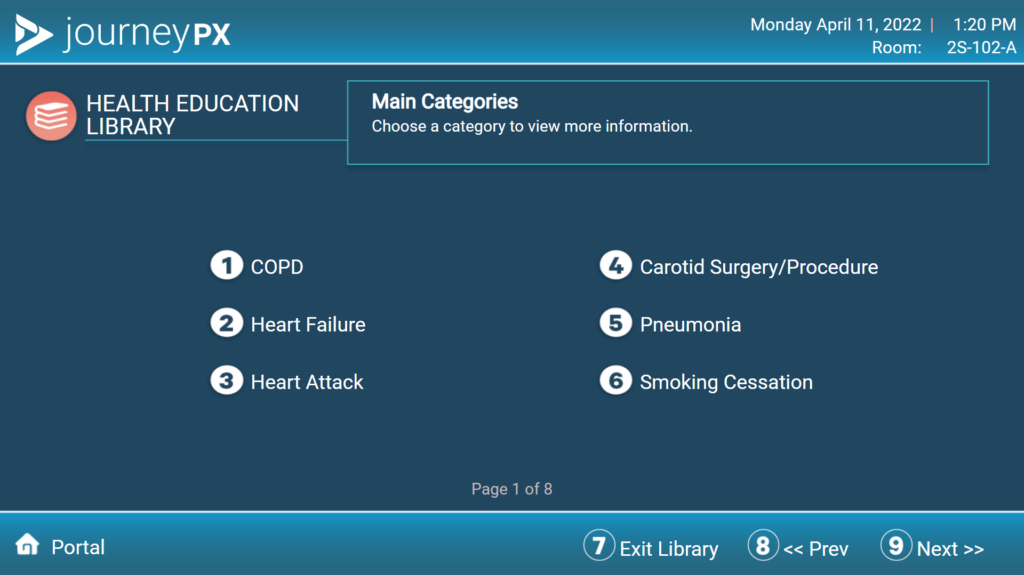
Journey PX: Streamlining Recovery
According to Godfrey, technology allows for a personalized approach to patient education. MDM Healthcare's cloud-based patient engagement platform, Journey PX, streamlines communication between patients and clinicians. Products like Journey PX's My Stay offer a helping hand to patients, empowering them with vital health education. With a large library of educational videos, patients are just a tap away from the answers. For more information about how Journey PX can help elevate your patient experience, schedule a free demo with us today.
Physical therapy plays a vital role in both healing and educating patients, serving as an integral component of a holistic approach to healthcare. By focusing on the body's natural ability to recover and adapt, physical therapists help patients regain mobility, reduce pain, and enhance overall well-being. Through personalized treatment plans, patients are not only guided through exercises and techniques to address specific conditions or injuries but are also empowered with knowledge about their own bodies. This education empowers individuals to take an active role in their healing process, fostering long-term health and preventive measures. In this way, physical therapy addresses not only the immediate physical concerns but also promotes a comprehensive understanding of one's health, ensuring a more holistic and sustainable approach to care. Utilizing technology, patients have the capability to access their treatment plans from the comfort of their own homes, empowering them to take charge of their own recovery.

For more insights on this topic, listen to the complete PX Space podcast interview below.